Because the distal 1/3 of the Achilles tendon is somewhat avascular, degeneration of the collagen matrix of the tendon is likely to occur in response to physical stress placed upon the tendon; this condition is called “Achilles tendinosus.” As compared to tendinitis, tendinosus is marked by a lack of inflammation. Tendinosus and tendinitis of the Achilles tendon often lead to one another. Further, degeneration of the tendinous tissue would increase the likelihood of an Achilles tendon rupture.
The paratenon is a loose connective tissue membrane of fascia that lies around the Achilles tendon and helps the tendon to slide along adjacent structures. With overuse, the paratenon can also become inflamed; this is termed “paratendinitis.”
There are two bursae that are located adjacent to the Achilles tendon. The subcutaneous bursa is located between the skin and tendon; the subtendinous bursa is located between the tendon and calcaneus. A bursa’s role is to decrease friction between two adjacent structures, in this case, the Achilles tendon and either the overlying skin or the underlying calcaneus. Excessive use of the Achilles tendon can cause bursitis. Another common cause is a rigid heel of a shoe that presses up against the skin over the Achilles tendon. Inflammation of either bursa in this region can be called “Achilles bursitis” or “retrocalcaneal bursitis.”
Chronic Achilles bursitis as well as tendinitis can result in enlargement of the calcaneal bone located adjacent to the bursa. This enlargement is known as a “pump bump;” it is named for the irritation that pumps, in other words high-heeled shoes, often cause to the region. When present, pump bumps can usually be palpated.
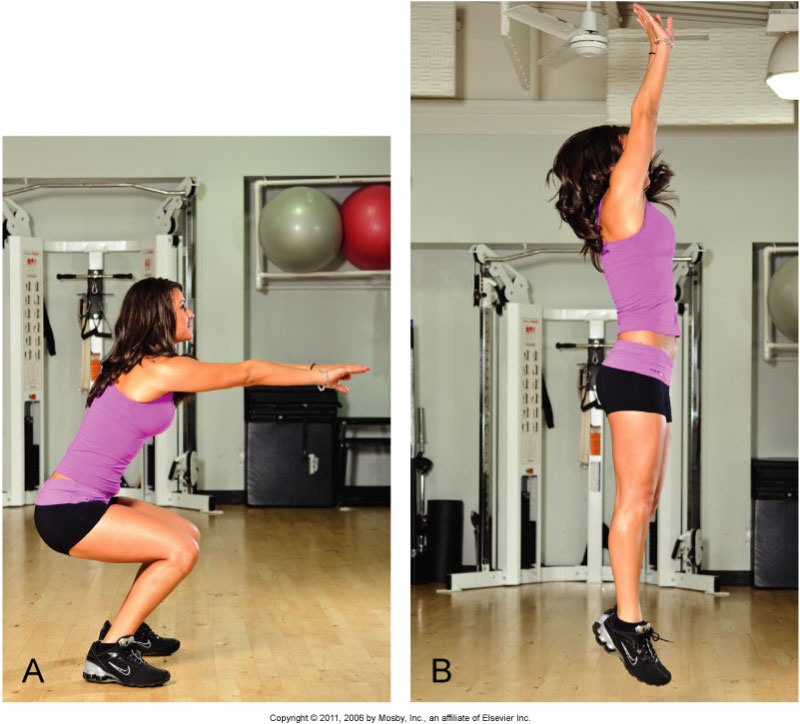
A squat jump in sports requires a strong contraction by plantarflexors, placing a strong tensile force on the Achilles tendon. Permission: Joseph E. Muscolino. Kinesiology: Skeletal Structure and Muscle Function, 3ed (2017), Elsevier.
Whereas Achilles tendinitis tends to occur due to chronic repeated microstresses placed on the Achilles tendon, Achilles tendon rupture more often occurs due to a sudden powerful macrostress placed on the tendon, usually plantarflexing powerfully to push the body forward. A typical example of this is approaching the net in tennis. As with Achilles’ tendinitis, lack of flexibility, insufficient warm up, increasing age, and degenerated collagen structure of tendinosus (perhaps aggravated by the use of anti-inflammatory medication) increase the chances of rupture. Certainly, a client with prior history of Achilles tendinitis or tendinosus is at an increased risk of rupture. Achilles tendon rupture occurs most often in middle-aged individuals because they are old enough that their tissues are not as elastic as they used to be, but young enough that they are active/athletic enough to place high demands on the tendon.